The RN Comfort Rest and Sleep Assessment is an indispensable tool for nurses, providing a systematic approach to assessing and addressing the comfort, rest, and sleep needs of patients. This assessment empowers nurses to identify and mitigate factors that hinder patient recovery and promote optimal patient outcomes.
The assessment encompasses key components such as pain, comfort, sleep quality, and environmental factors, ensuring a holistic evaluation of patient well-being. Nurses play a pivotal role in administering the assessment, obtaining accurate data, and interpreting the results to develop individualized interventions.
Introduction to RN Comfort Rest and Sleep Assessment
The RN Comfort Rest and Sleep Assessment is a comprehensive tool designed to evaluate the comfort, rest, and sleep patterns of patients in a healthcare setting. It is an essential component of nursing care, as it provides valuable insights into the patient’s overall well-being and quality of life.
The assessment tool consists of several components, including:
- Patient demographics and medical history
- Assessment of the patient’s physical comfort, including pain, fatigue, and mobility
- Assessment of the patient’s sleep patterns, including duration, quality, and disturbances
- Assessment of the patient’s environment, including factors that may affect comfort, rest, and sleep
Significance of RN Comfort Rest and Sleep Assessment
The RN Comfort Rest and Sleep Assessment is significant for several reasons:
- It helps nurses identify and address factors that may be affecting the patient’s comfort, rest, and sleep.
- It provides a baseline for monitoring the patient’s progress over time.
- It facilitates communication between nurses and other healthcare professionals involved in the patient’s care.
- It contributes to the development of individualized care plans that promote the patient’s comfort, rest, and sleep.
Components of the Assessment
The RN Comfort Rest and Sleep Assessment is a comprehensive tool designed to assess key factors that influence patient comfort, rest, and sleep. By evaluating these components, healthcare professionals can develop individualized interventions to improve patient outcomes.
The assessment includes the following key components:
- Pain
- Comfort
- Sleep quality
- Environmental factors
Pain
Pain is a subjective experience that can significantly impact patient comfort and sleep. The assessment includes questions about the presence, location, intensity, and duration of pain. By understanding the nature of the pain, healthcare professionals can determine appropriate pain management strategies.
Comfort
Comfort refers to the patient’s physical and emotional well-being. The assessment evaluates factors such as positioning, mobility, and skin integrity. Identifying areas of discomfort can help healthcare professionals optimize patient positioning, provide support devices, and prevent pressure injuries.
Sleep quality
Sleep quality is essential for overall health and well-being. The assessment includes questions about sleep patterns, duration, and quality. By assessing sleep quality, healthcare professionals can identify potential sleep disturbances and develop interventions to improve sleep hygiene.
Environmental factors
Environmental factors can significantly influence patient comfort and sleep. The assessment evaluates factors such as temperature, noise, and lighting. By optimizing the patient’s environment, healthcare professionals can create a conducive atmosphere for rest and sleep.
Implementation and Administration
Implementing the RN Comfort, Rest, and Sleep Assessment in a clinical setting involves a structured process and clear delineation of roles and responsibilities.
Nurses play a pivotal role in administering the assessment, ensuring accurate and reliable data collection. They are responsible for:
- Familiarizing themselves with the assessment tool and its components.
- Approaching patients in a sensitive and empathetic manner, establishing a rapport that encourages open and honest responses.
- Administering the assessment in a private and comfortable setting, free from distractions.
- Using active listening skills to elicit detailed and comprehensive responses from patients.
- Documenting the assessment findings accurately and thoroughly, capturing both subjective and objective data.
- Communicating the assessment results to other members of the healthcare team, facilitating a collaborative approach to patient care.
Obtaining accurate and reliable data is essential for the assessment to be effective. Nurses should:
- Use standardized assessment tools with established validity and reliability.
- Train healthcare providers on the proper administration of the assessment.
- Provide clear instructions to patients, ensuring they understand the purpose and importance of the assessment.
- Minimize bias and subjectivity by using objective measures and rating scales.
- Regularly review and update the assessment tool to ensure it remains current and relevant to clinical practice.
Interpretation of Results

Interpreting the results of the RN Comfort Rest and Sleep Assessment involves analyzing the collected data to identify patterns, trends, and potential areas of concern related to the patient’s comfort, rest, and sleep. This assessment provides valuable insights into the patient’s subjective experiences, enabling healthcare professionals to develop individualized care plans that address their specific needs.
Scoring Systems and Evaluation Methods
Various scoring systems and evaluation methods can be employed to interpret the assessment findings. These tools assist in quantifying and standardizing the data, facilitating comparisons over time and between patients. Common scoring systems include:
- Numeric Rating Scale (NRS):A simple and widely used scale where patients rate their comfort, rest, or sleep on a scale of 0 to 10, with 0 indicating “no discomfort/rest/sleep” and 10 indicating “worst possible discomfort/rest/sleep.”
- Visual Analogue Scale (VAS):A horizontal line where patients mark a point that corresponds to their level of discomfort, rest, or sleep. The distance from the left end of the line to the marked point represents the score.
- Comfort Assessment Scale (CAS):A more comprehensive scale that evaluates multiple aspects of comfort, including physical, psychological, and environmental factors.
Other evaluation methods include:
- Narrative analysis:Examining the patient’s written or verbal responses to open-ended questions, providing qualitative insights into their experiences.
- Trend analysis:Comparing the patient’s scores over time to identify changes or patterns that may indicate improvements or areas for further intervention.
Interventions and Management
Interventions to improve patient comfort, rest, and sleep are crucial for promoting overall well-being and recovery. These interventions should be evidence-based and tailored to the individual needs of the patient.
There are numerous evidence-based interventions that can be implemented to improve patient comfort, rest, and sleep. These interventions can be categorized into non-pharmacological and pharmacological approaches.
Non-Pharmacological Interventions
- Environmental modifications: Creating a conducive environment for sleep, such as maintaining a cool, dark, and quiet room.
- Cognitive-behavioral therapy (CBT): A type of therapy that helps patients identify and change negative thoughts and behaviors that interfere with sleep.
- Relaxation techniques: Practicing relaxation techniques, such as deep breathing, meditation, or yoga, can help reduce stress and promote sleep.
- Light therapy: Exposure to bright light during the day and darkness at night can help regulate the body’s natural sleep-wake cycle.
- Exercise: Regular physical activity can improve sleep quality, but it should be avoided close to bedtime.
- Sleep hygiene education: Providing patients with education on healthy sleep habits and the importance of good sleep hygiene.
Pharmacological Interventions
- Sedatives and hypnotics: These medications can help induce sleep, but they should be used with caution and for short-term use only.
- Melatonin: A hormone that helps regulate the body’s natural sleep-wake cycle. Melatonin supplements may be helpful for people with sleep disorders.
- Antidepressants: Certain antidepressants, such as trazodone and mirtazapine, have sedative effects and may be helpful for people with sleep problems.
The choice of intervention will depend on the underlying cause of the patient’s sleep problems and their individual needs. It is important to work closely with a healthcare professional to determine the most appropriate interventions for each patient.
Evaluation and Outcomes: Rn Comfort Rest And Sleep Assessment
Evaluating the effectiveness of interventions implemented based on the assessment findings is crucial to ensure optimal patient outcomes. It helps identify areas where adjustments are needed to improve the quality of care.
Regular tracking of patient outcomes is essential for evaluating the effectiveness of interventions. This includes monitoring sleep patterns, pain levels, anxiety levels, and overall well-being. Tracking can be done through patient self-reporting, nursing observations, or objective measures such as actigraphy or polysomnography.
Methods for Making Necessary Adjustments
Based on the evaluation findings, adjustments to the care plan may be necessary to enhance the effectiveness of interventions. This may involve modifying existing interventions, introducing new ones, or discontinuing those that are not yielding desired results.
- Modify Existing Interventions:Adjust the frequency, duration, or intensity of an intervention based on patient response.
- Introduce New Interventions:Implement additional interventions that address specific needs or concerns identified during the evaluation.
- Discontinue Ineffective Interventions:Remove interventions that are not contributing to the desired outcomes or may be causing adverse effects.
Education and Resources
Nurses play a crucial role in educating patients and families about comfort, rest, and sleep. They provide information about the importance of sleep, the factors that can affect sleep, and the strategies that can be used to improve sleep quality.
Nurses also provide information about available resources and support systems for patients experiencing sleep disturbances. These resources may include sleep clinics, support groups, and online resources.
Available Resources
There are a number of resources available to help patients improve their sleep. These resources include:
- Sleep clinics: Sleep clinics are specialized centers that provide diagnosis and treatment for sleep disorders.
- Support groups: Support groups can provide patients with a sense of community and support. They can also provide information about sleep disorders and treatment options.
- Online resources: There are a number of online resources available to help patients improve their sleep. These resources include websites, blogs, and apps.
Special Considerations

RN Comfort Rest and Sleep Assessment may require modifications to accommodate the unique needs of specific patient populations, including older adults, children, and those with cognitive impairments.
Adapting the assessment and interventions to meet these unique needs is crucial for effective pain management and improving patient outcomes.
Older Adults
- Physiological Changes:Older adults may experience physiological changes that affect sleep, such as decreased melatonin production and increased sleep fragmentation.
- Cognitive Impairments:Cognitive impairments, such as dementia, can impact the ability to communicate sleep-related concerns and may require alternative assessment methods.
- Polypharmacy:Older adults often take multiple medications, which can have side effects that interfere with sleep.
- Environmental Factors:Environmental factors, such as noise and light, can disrupt sleep in older adults.
Children
- Developmental Stage:Children’s sleep patterns change as they develop, and the assessment should be tailored to their developmental stage.
- Parental Involvement:Parents or caregivers play a significant role in providing information about the child’s sleep habits.
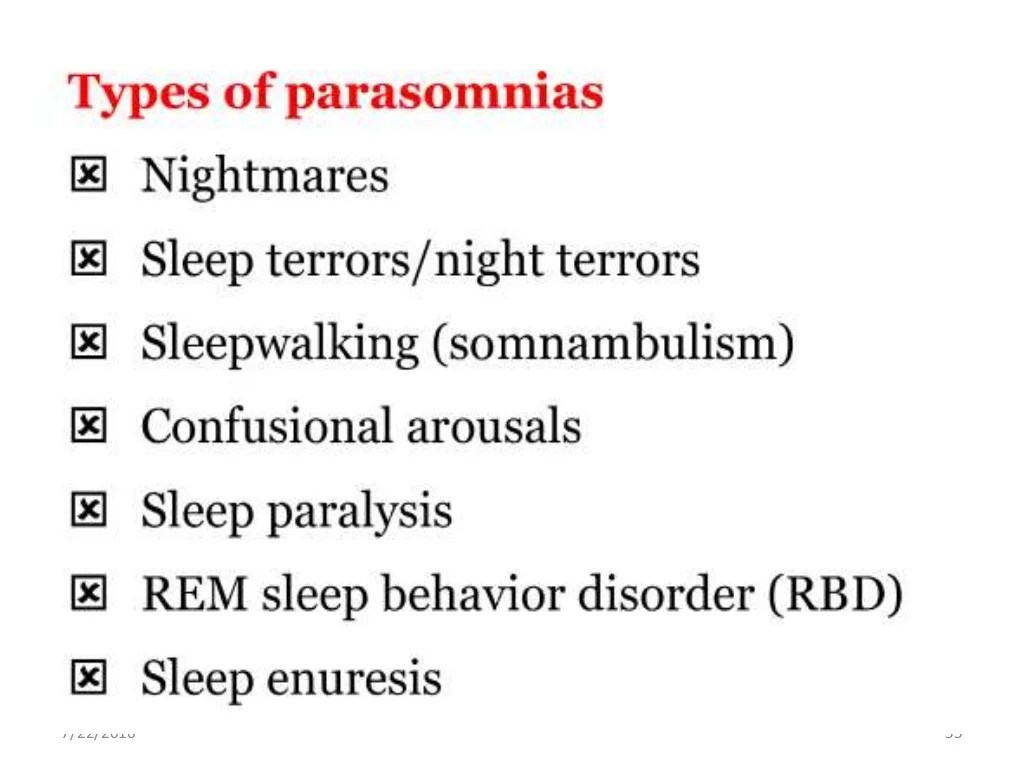
- Behavioral Issues:Behavioral issues, such as bedtime resistance or nightmares, can impact sleep in children.
- Medical Conditions:Medical conditions, such as asthma or allergies, can affect sleep in children.
Cognitive Impairments
- Communication Difficulties:Individuals with cognitive impairments may have difficulty communicating their sleep-related concerns.
- Assessment Modifications:Alternative assessment methods, such as observation or behavioral mapping, may be necessary.
- Non-Verbal Cues:Non-verbal cues, such as facial expressions or body language, can provide valuable information about sleep disturbances.
- Caregiver Involvement:Caregivers can provide valuable information about the individual’s sleep patterns and behaviors.
Future Directions and Research
The RN Comfort Rest and Sleep Assessment (RN-CRSA) is a valuable tool for assessing comfort, rest, and sleep in hospitalized patients. As the field of nursing and healthcare continues to evolve, it is important to consider future directions and research related to this assessment.
Potential Advancements in the Assessment Tool
- Integration of Technology:Exploring the use of mobile apps or electronic health records (EHRs) to enhance the efficiency and accuracy of the assessment process.
- Development of Subscales:Investigating the feasibility of creating subscales within the RN-CRSA to measure specific aspects of comfort, rest, and sleep, such as pain, anxiety, or environmental factors.
- Validation in Diverse Populations:Conducting studies to validate the RN-CRSA in different patient populations, including those with specific conditions or cultural backgrounds, to ensure its generalizability.
Application in Clinical Practice
- Development of Clinical Pathways:Utilizing the RN-CRSA to develop clinical pathways that guide nurses in providing individualized interventions to improve patient comfort, rest, and sleep.
- Evaluation of Interventions:Conducting research to evaluate the effectiveness of interventions based on the RN-CRSA findings, such as sleep hygiene education or pain management strategies.
- Integration into Quality Improvement Initiatives:Incorporating the RN-CRSA into quality improvement initiatives to monitor and improve patient outcomes related to comfort, rest, and sleep.
Common Queries
What are the key components of the RN Comfort Rest and Sleep Assessment?
The key components include pain, comfort, sleep quality, and environmental factors.
How do nurses interpret the results of the assessment?
Nurses use scoring systems and other methods to evaluate the findings and identify patient needs.
What are some evidence-based interventions for improving patient comfort, rest, and sleep?
Interventions include pain management, environmental modifications, and relaxation techniques.